Internist Gail Povar has many female patients making their way through menopause, some having a tougher time than others. Several women with similar stories stand out in her mind. Each came to Povar’s Silver Spring, Md., office within a year or two of stopping her period, complaining of frequent hot flashes and poor sleep at night. “They just felt exhausted all the time,” Povar says. “The joy had kind of gone out.”
And all of them “were just absolutely certain that they were not going to take hormone replacement,” she says. But the women had no risk factors that would rule out treating their symptoms with hormones. So Povar suggested the women try hormone therapy for a few months. “If you feel really better and it makes a big difference in your life, then you and I can decide how long we continue it,” Povar told them. “And if it doesn’t make any difference to you, stop it.”
At the follow-up appointments, all of these women reacted the same way, Povar recalls. “They walked in beaming, absolutely beaming, saying, ‘I can’t believe I didn’t do this a year ago. My life! I’ve got my life back.’ ”
That doesn’t mean, Povar says, that she’s pushing hormone replacement on patients. “But it should be on the table,” she says. “It should be part of the discussion.”
Hormone replacement therapy toppled off the table for many menopausal women and their doctors in 2002. That’s when a women’s health study, stopped early after a data review, published results linking a common hormone therapy to an increased risk of breast cancer, heart disease, stroke and blood clots. The trial, part of a multifaceted project called the Women’s Health Initiative, or WHI, was meant to examine hormone therapy’s effectiveness in lowering the risk of heart disease and other conditions in women ages 50 to 79. It wasn’t a study of hormone therapy for treating menopausal symptoms.
But that nuance got lost in the coverage of the study’s results, described at the time as a “bombshell,” a call to get off of hormone therapy right away. Women and doctors in the United States heeded the call. A 2012 study in Obstetrics & Gynecology showed that use plummeted: Oral hormone therapy, taken by an estimated 22 percent of U.S. women 40 and older in 1999–2000, was taken by fewer than 12 percent of women in 2003–2004. Six years later, the number of women using oral hormone therapy had sunk below 5 percent.
Specialists in women’s health say it’s time for the public and the medical profession to reconsider their views on hormone therapy. Research in the last five years, including a long-term follow-up of women in the WHI, has clarified the risks, benefits and ideal ages for hormone therapy. Medical organizations, including the Endocrine Society in 2015 and the North American Menopause Society in 2017, have released updated recommendations. The overall message is that hormone therapy offers more benefits than risks for the relief of menopausal symptoms in mostly healthy women of a specific age range: those who are under age 60 or within 10 years of stopping menstruation.
“A generation of women has missed out on effective treatment because of misinformation,” says JoAnn Pinkerton, executive director of the North American Menopause Society and a gynecologist who specializes in menopause at the University of Virginia Health System in Charlottesville. It’s time to move beyond 2002, she says, and have a conversation based on “what we know now.”
End of an era
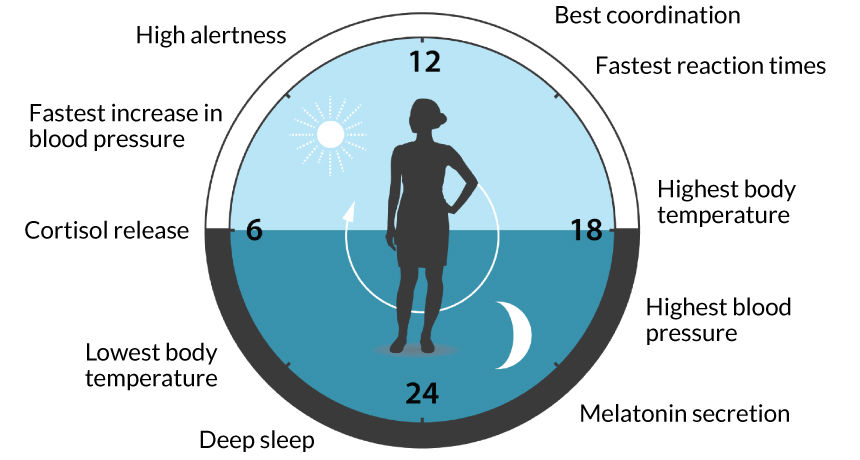
Menopause, the final menstrual period, signals the end of fertility and is confirmed after a woman has gone 12 months without having a period. From then on she is postmenopausal. Women reach menopause around age 51, on average. In the four to eight years before, called perimenopause, the amount of estrogen in the body declines as ovarian function winds down. Women may have symptoms related to the lack of estrogen beginning in perimenopause and continuing after the final period.
Probably the best-known symptom is the hot flash, a sudden blast of heat, sweating and flushing in the face and upper chest. These temperature tantrums can occur at all hours. At night, hot flashes can produce drenching sweats and disrupt sleep.
Hot flashes arise because the temperature range in which the body normally feels comfortable narrows during the menopause transition, partly in response to the drop in estrogen. Normally, the body takes small changes in core body temperature in stride. But for menopausal women, the slightest uptick in degree can be a trigger for the vessels to dilate, which increases blood flow and sweating.
About 75 to 80 percent of menopausal women experience hot flashes and night sweats, on and off, for anywhere from a couple of years to more than a decade. In a study in JAMA Internal Medicine in 2015, more than half of almost 1,500 women enrolled at ages 42 to 52 reported frequent hot flashes — occurring at least six days in the previous two weeks — with symptoms lasting more than seven years.
A sizable number of women have moderate or severe hot flashes, which spread throughout the body and can include profuse sweating, heart palpitations or anxiety. In a study of 255 menopausal women, moderate to severe hot flashes were most common, occurring in 46 percent of women, during the two years after participants’ last menstrual period. A third of all the women still experienced heightened hot flashes 10 years after menopause, researchers reported in 2014 in Menopause.
Besides hot flashes and night sweats, roughly 40 percent of menopausal women experience irritation and dryness of the vulva and vagina, which can make sexual intercourse painful. These symptoms tend to arise after the final period.
Alarm bells
In the 1980s and ’90s, researchers observed that women using hormone therapy for menopausal symptoms had a lower risk of heart disease, bone fractures and overall death. Some doctors began recommending the medication not just for symptom relief, but also for disease prevention.
Observational studies of the apparent health benefits of hormone therapy spurred a more stringent study, a randomized controlled trial, which tested the treatment’s impact by randomly assigning hormones to some volunteers and not others. The WHI hormone therapy trials assessed heart disease, breast cancer, stroke, blood clots, colorectal cancer, hip fractures and deaths from other causes in women who used the hormones versus those who took a placebo. Two commonly prescribed formulations were tested: a combined hormone therapy — estrogen sourced from horses plus synthetic progesterone — and estrogen alone. (Today, additional U.S. Food and Drug Administration–approved formulations are available.)
The 2002 WHI report in JAMA, which described early results of the combined hormone therapy, shocked the medical community. The study was halted prematurely because after about five years, women taking the hormones had a slightly higher risk of breast cancer and an overall poor risk-to-benefit ratio compared with women taking the placebo. While the women taking hormones had fewer hip fractures and colorectal cancers, they had more breast cancers, heart disease, blood clots and strokes. The findings were reported in terms of the relative risk, the ratio of how often a disease happened in one group versus another. News of a 26 percent increase in breast cancers and a 41 percent increase in strokes caused confusion and alarm.
Women dropped the hormones in droves. From 2001 to 2009, the use of all hormone therapy among menopausal women, as reported by physicians based on U.S. office visits, fell 52 percent, according to a 2011 study in Menopause.
But, researchers say, the message that hormone therapy was bad for all was unwarranted. “The goal of the WHI was to evaluate the balance of benefits and risks of menopausal hormone therapy when used for prevention of chronic disease,” says JoAnn Manson, a physician epidemiologist at Harvard-affiliated Brigham and Women’s Hospital in Boston and one of the lead investigators of the WHI. “It was not intended to evaluate its role in managing menopausal symptoms.”
Along with the focus on prevention, the WHI hormone therapy trials were largely studies of older women — in their 60s and 70s. Only around one-third of participants started the trial between ages 50 and 59, the age group more likely to be in need of symptom relief. Hormone therapy “was always primarily a product to use in women entering menopause,” says Howard Hodis, a physician scientist who focuses on preventive medicine at the University of Southern California’s Keck School of Medicine in Los Angeles. “The observational studies were based on these women.”
Also lost in the coverage of the 2002 study results was the absolute risk, the actual difference in the number of cases of disease between two groups. The group on combined hormone therapy had eight more cases of breast cancer per 10,000 women per year than the group taking a placebo. Hodis notes that that absolute risk translates to less than one extra case for every 1,000 women, which is classified as a rare risk by the Council for International Organizations of Medical Sciences, a World Health Organization group. There was also less than one additional case for every 1,000 women per year for heart disease and for stroke in the hormone-treated women compared with those on placebo.
In 2004, researchers published results of the WHI study of estrogen-only therapy, taken for about seven years by women who had had their uteruses surgically removed. (Progesterone is added to hormone therapy to protect the uterus lining from a risk of cancer seen with estrogen alone.) The trial, also stopped early, reported a decreased risk of hip fractures and breast cancer, but an increased risk of stroke. The study didn’t change the narrative that hormone therapy wasn’t safe.
Timing is everything
Since the turn away from hormone therapy, follow-up studies have brought nuance not initially captured by the first two reports. Researchers were finally able to tease out the results that applied to “the young women — and I love saying this — young women 50 to 59 who are most apt to present with symptoms of menopause,” says Cynthia Stuenkel, an internist and endocrinologist at the University of California, San Diego School of Medicine in La Jolla.
In 2013, Manson and colleagues reported data from the WHI grouped by age. It turned out that absolute risks were smaller for 50- to 59-year-olds than they were for older women, especially those 70 to 79 years old, for both combined therapy and estrogen alone. For example, in the combined hormone therapy trial, treated 50- to 59-year-olds had five additional cases of heart disease and five more strokes per 10,000 women annually compared with the same-aged group on placebo. But the treated 70- to 79-year-olds had 19 more heart disease cases and 13 more strokes per 10,000 women annually than women of the same age taking a placebo. “So a lot more of these events that were of concern were in the older women,” Stuenkel says.
Story continues below graphs
A Danish study reported in 2012 of about 1,000 recently postmenopausal women, ages 45 to 58, also supported the idea that timing of hormone treatment matters. The randomized controlled trial examined the use of different formulations of estrogen (17β-estradiol) and progesterone than the WHI. The researchers reported in BMJ that after 10 years, women taking hormone therapy — combined or estrogen alone — had a reduced risk of mortality, heart failure or heart attacks, and no added risk of cancer, stroke or blood clots compared with those not treated.
These findings provide evidence for the timing hypothesis, also supported by animal studies, as an explanation for the results seen in younger women, especially in terms of heart disease and stroke. In healthy blood vessels, more common in younger women, estrogen can slow the development of artery-clogging plaques. But in vessels that already have plaque buildup, more likely in older women, estrogen may cause the plaques to rupture and block an artery, Manson explains.
Recently, Manson and colleagues published a long-term study of the risk of death in women in the two WHI hormone therapy trials — combined therapy and estrogen alone — from the time of trial enrollment in the mid-1990s until the end of 2014. Use of either hormone therapy was not associated with an added risk of death during the study or follow-up periods due to any cause or, specifically, death from heart disease or cancer, the researchers reported in JAMA in September 2017. The study provides reassurance that taking hormone therapy, at least for five to seven years, “does not show any mortality concern,” Stuenkel says.
Both the Endocrine Society and the North American Menopause Society state that, for symptom relief, the benefits of FDA-approved hormone therapy outweigh the risks in women younger than 60 or within 10 years of their last period, absent health issues such as a high risk of breast cancer or heart disease. The menopause society position statement adds that there are also benefits for women at high risk of bone loss or fracture.
Today, the message about hormone therapy is “not everybody needs it, but if you’re a candidate, let’s talk about the pros and cons, and let’s do it in a science-based way,” Pinkerton says.
Hormone therapy is the most effective treatment for hot flashes, night sweats and genital symptoms, she says. A review of randomized controlled trials, published in 2004, reported that hormone therapy decreased the frequency of hot flashes by 75 percent and reduced their severity as well.
More than 50 million U.S. women will be older than 51 by 2020, Manson says. Yet today, many women have a hard time finding a physician who is comfortable prescribing hormone therapy or even just managing a patient’s menopausal symptoms, she says.
Stuenkel, who says many younger doctors stopped learning about hormone therapy after 2002, is trying to play catch up. When she teaches medical students and doctors about treating menopausal symptoms, she brings up three questions to ask patients. First, how bothersome are the symptoms? Some women say “fix it, get me through the day and the night, put me back in order,” Stuenkel says. Other women’s symptoms are not as disruptive. Second, what does the patient want? Third, what is safe for this particular woman, based on her health? If a woman’s health history doesn’t support the use of hormone therapy, or she just isn’t interested, there are nonhormonal options, such as certain antidepressants, and also nondrug lifestyle approaches.
Menopause looms large for many women, Povar says, and discussing a patient’s expectations as well as whether hormone therapy is the right approach becomes a unique discussion with each patient, she says. “This is one of the most individual decisions a woman makes.”